Welcome to our Clerkship Resource page. Additional information can be found in the Clerkship Guidebook, published by Doctors Manitoba, with the help of students. This is the most comprehensive clerkship resource available.
Class of 2026 Council Directory
| President | Riley Seirhuis |
| Academic Representative | Ben Meyers Lucas Mosienko |
| Sports Rep | Caitlin Le Diana Prince |
| Social Representative | Thomas Manuel Sam Narvey |
| Wellness Representative | Michaela Groen Parth Saul |
| Secretary | Shoshana Cook-Libin |
| Treasurer | Guneet Uppal Umema Rafay |
| Yearbook Committee | Cynthia James Orest Fylyma Morgan Wokes |
| Local Officer of Indigenous Health | Connor Roque |
| Global Health Liaison Junior | Jun Kim |
Class of 2025 Council Directory
| President | Jayelle Friesen-Enns |
| Academic Representative | Connor Ford Mehrin Ahmed |
| Secretary | Lisa Kim |
| Treasurer | Christine Kennedy Ben Borys |
| Social Representative | Anmolpreet Mann Daniel Lee |
| Yearbook Committee | Rachel Willim Mehrin Ahmed Alex Chin |
| Wellness Representative | Bobby Mcnair Amanda Wong |
Overview
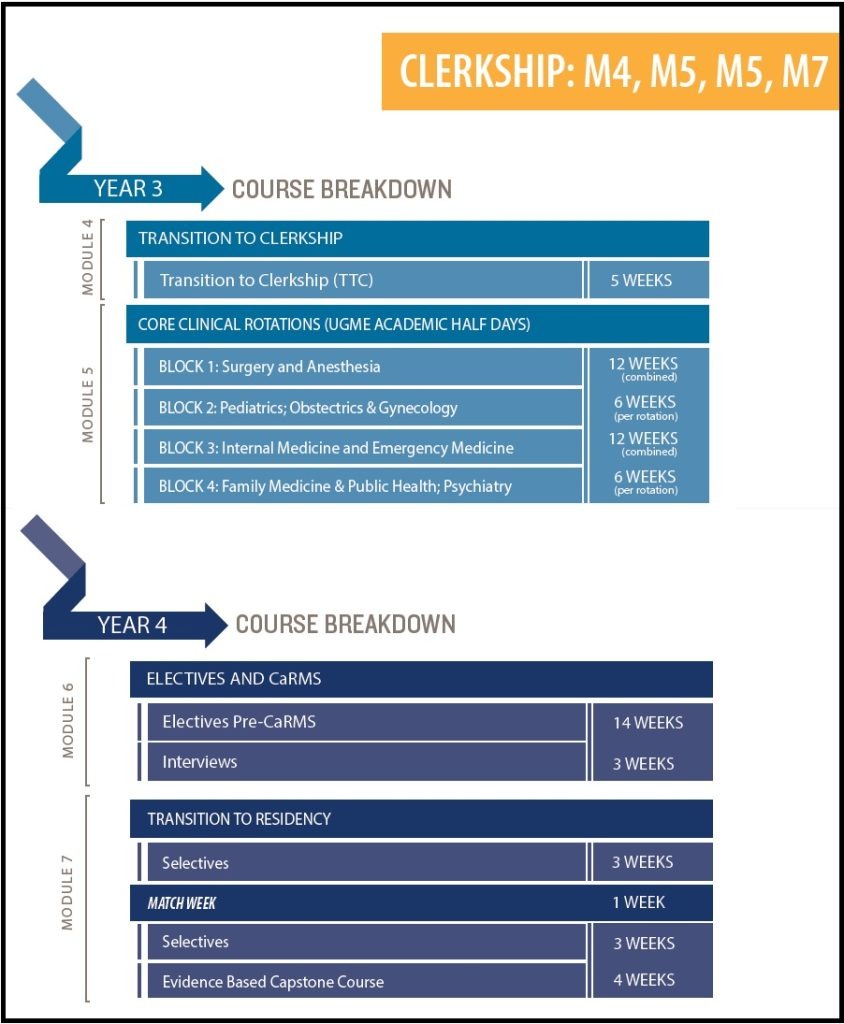
Clerkship is a two year process that serves to refine students’ medical knowledge and interpersonal skills using hands-on learning and experience.
Year 3 begins with M4 – Transition to Clerkship, a 3 week period that serves to acclimate students to the clinical duties and scenarios that they will soon find themselves in by incorporating tutorials, simulations, and real patient encounters.
Students are divided into 8 tracks to rotate through M5 – Core Clinical Rotations.
The Surgery and Anesthesia block provides clinical teaching in:
- General Surgery (3 wks)
- Musculoskeletal medicine (2 wks)
- A Surgical subspecialty (2 wks)
- Anesthesia (2 wks)
The Pediatrics and Obstetrics & Gynecology block provides clinical teaching in:
- Pediatrics inpatient care (3 wks)
- Pediatric outpatient care (3 wks)
- Obstetrics (2 wks)
- Gynecology (2 wks)
- Obstetrics & gynecology outpatient clinics (2 wks)
The Internal Medicine and Emergency Medicine block provides clinical teaching in:
- Internal medicine CTU (6 wks)
- Internal medicine subspecialty (2 wks)
- Emergency medicine (4 wks)
The Psychiatry and Family Medicine/Public Health block provides clinical teaching in:
- Psychiatry (inpatient, outpatient and consultations – 6 wks)
- Rural family medicine clinic (5 wks)
- Public health (1 wk)
See this spreadsheet for tips and info about various rotations and Selectives and feel free to add your own experiences!
Core rotations are followed by M6 – Electives and CaRMS. Students have 14 weeks of elective rotations, which must include at least three different disciplines. During this time, students also work on their CaRMS applications in preparation for the 3 week CaRMS Interview period. This module closes with the CCE, an OSCE-style examination in the simulation lab.
The medical school experience ends with M7 – Transition to Residency, in which students are provided with more opportunities to enhance their skills before residency begins. This includes two 3-week blocks of selectives intended emphasize community and outpatient activities. Sandwiched between the two selective blocks is Match week – a week focusing on team building, leadership, and what to expect in the coming years. Additionally, students are given the day off to celebrate on Match Day day. There are also formal teaching sessions each Friday afternoon throughout the selective blocks, culminating in a written paper and presentation in the seventh week. The year concludes with a comprehensive course review and an ACLS course to aid students in preparing for the MCCQE Pt I.
Selecting Your Track
Students in Year 2 are given the opportunity to request specific “Clerkship Tracks”; i.e. which order they will experience their core rotations. This typically occurs near the end of Winter/beginning of Spring. We encourage students to seek out mentors in upper years for advice regarding the advantages and disadvantages of each Track. Some general topics to consider:
- Rotating through disciplines you are “on the fence” about early, in order to evaluate career interest
- Rotating through disciplines you are keen on later on, in order to better impress attendings/residents
Clerkship Evaluations
Each rotation will have:
- MITER (Mid-point In-Training Evaluation Report) – At the mid-point of each rotation, students score themselves on entrada in key performance areas and write comments about their strengths and weaknesses. The MITER is then discussed with one of your preceptors or the rotation head. MITERs are formative and rotations that are shorter than 4 weeks have a FITER only.
- FITER (Final In-Training Evaluation Report) – At the end of each rotation, preceptors or rotation heads fill out the same report about each student and discuss it with them. FITERs yield the overall Pass/Borderline Pass/Fail grade for the rotation as a whole. The comments from your FITER appear on your Medical Student Performance Record (MSPR), which programs view for CaRMS. The MSPR does not show your numerical scores from your rotations.
- Essential Clinical Presentations (ECPs) – A list of patient symptoms and medical procedures that you must be exposed to over the course of the rotation. These are tracked in your logbook on entrada.
- NBME Examinations – Surgery, Pediatrics, Obstetrics/Gynecology, Internal Medicine, Family Medicine, and Psychiatry each conclude with an online multiple choice examination. These tests are pass/fail, with a passing grade designated as the 11th percentile nationally. An NBME failure does not constitute a rotation failure, and vice-versa – they are mutually exclusive. Only pass/fail appears on your MSPR, not your numerical score.
Maps
Call Shifts
- Each rotation has different call requirements, with schedules made by senior residents or other departmental coordinators weeks in advance. If there is a specific date that you will not be able to take call, it is good practice to contact the department administrator at least 6 weeks before your rotation with this information.
- If your call schedule has already been made and there is a conflict, you may attempt to trade shifts with other students/residents at the discretion of the schedule coordinator.
- If you’re on call for at least 8 hours of a statutory holiday, you are allowed one additional post-call day with the caveat that it has to be taken during the rotation the stat occurred. Emergency Dept shifts on stat days do not count as you’re not “on call”.
Absences
- For anticipated leaves, fill in UGME’s absence form. It must be submitted at least 6 weeks in advance and supporting documentation must be included. Requests for leave are not automatically granted so do not make travel arrangements without getting approval first.
- If you do have an absence approved from the clerkship director and program, it is your responsibility to let your service know. Good practice is to let them know in advance and a reminder the day before your LOA starts. The chief residents making your call schedule may not always be informed/aware of your LOA. On some services, the chief resident will ask you in advance if you have any specific dates that you’d like off. Let them know at this time. As mentioned earlier, if a call shift has been scheduled it is best to find a student/resident on the service to switch with.
- For shorter anticipated absences (e.g. a doctor’s appointment or other personal meeting), an official LOA is not required. Simply speak with your supervisor and then email the administrative assistant of the affected rotation to coordinate. Recurring appointments may require completion of the LOA form, however.
- There is no tolerance for unapproved absences during clerkship – failure to obtain approval constitutes a failure of professional responsibility. For the full attendance policy, click here.
- In the case of unanticipated absences (e.g. car accidents) – be sure to contact your direct supervisor as soon as possible to appraise them of the situation. It is also good practice to contact the UGME office as well. If you need more than 2 days off for an illness, a medical certificate will need to be submitted to UGME.
- Students may not miss >25% of any given rotation, regardless of the reason, without penalty of repeating the rotation
- There is a limit of 6 LOAs per year.
Wellness and Mistreatment
Medical School can be incredibly challenging but it should also be a positive and rewarding experience. You can’t properly learn or care for others if you don’t first care for yourself.
If you have any concerns regarding mistreatment or safety during your clerkship, you are encouraged to address it personally with the relevant Clerkship Rotation Head. If you’d prefer, you can speak with a student representative (e.g. from the MMSA Exec or your Class Council), who can address the issue on your behalf, or you can submit an online mistreatment report. For more information, read the College’s Policy for Prevention of Learner Mistreatment.
Be sure to also take a look at our Wellness page for tips about personal wellness. When in doubt, contact Dr. Aviva Goldberg, Dean of Student Affairs – she’s the best! As mentioned above, we at the MMSA are also here for you – please feel free to drop us a line anytime if you’d like to speak with a peer.
Electives and CaRMS
As medical students ourselves, we do not profess to know any secrets to the electives or CaRMS processes. However, we do have a few ideas regarding good practices:
- Do everything early, as you never know when something will pop up! Try to make a wishlist schedule and register for the AFMC Portal in December/January of Year 3. Ask for references on each rotation as you go. Start working on your CV and personal letters before CaRMS applications even open.
- Try to connect with mentors at different stages of practice. What do residents have to say about their program/field? How about earlier versus more senior attendings?
- Use the available resources! Student Affairs and Doctors Manitoba have a lot to offer.
- Keep a journal – this can help you to remember important experiences and stories for interviews and career decisions.
- Practice with your peers! Their feedback will be invaluable, as will the insight you gain as a mock interviewer.
General Tips
- Dress and act professionally.
- The Golden Rule – treating others poorly can come back to haunt you no matter who it is! Plus it’s just not very nice.
- Ask questions – our job is to learn and there’s no such thing as a stupid question.
- JOURNAL. Write down your experiences throughout the year. You’ll end up with a goldmine of interesting anecdotes and concrete examples to draw from for CaRMS interviews.
- Volunteer to do tasks to make things easier for others – that being said, be sure to let your supervisor know if you’re feeling that your role has become too menial.
- Make time for your hobbies – keeping up with the things you enjoy outside of medicine is crucial to maintaining balance.
- Sleep more. You deserve it.
