Welcome to our Pre-clerkship Resource page. Please click the tabs below to find out more information. You can access the recently completed pre-clerkship survival guide from Doctors Manitoba. It’s full of tips and tricks that can help you through your first two years of med school and beyond!
Class of 2028 Council Directory
| President | |
| Academic Representatives | |
| Sports Representative | |
| Social Representative | |
| Wellness Representative | |
| Secretary | |
| Treasurer | |
| Yearbook Committee | |
| Local Officer of Indigenous Health | |
| BSc Med Representative | |
| MMSA Med 1 Representative | |
| Community Outreach Representative | |
| Global Health Liaison Jr |
Class of 2027 Council Directory
| President | |
| Academic Representatives | |
| Sports Representatives | |
| Social Representatives | |
| Wellness Representatives | |
| Secretary | |
| Treasurer | |
| Yearbook Committee | |
| Local Officer of Indigenous Health | |
| BSc Med Rep | |
| MMSA Med 1 Representative | |
| Community Outreach Representative | |
| Global Health Liaison Jr |
Pre-clerkship Curriculum
Overview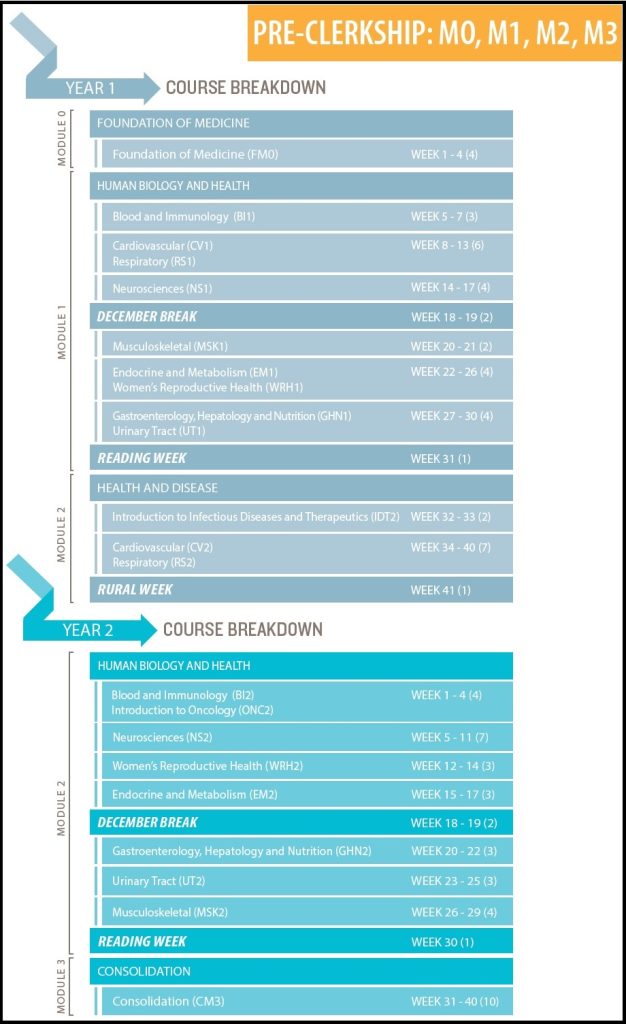
An entirely new pre-clerkship curriculum was introduced in 2014. It is separated into 4 Modules (M0-M3) spread throughout the first and second years of Medical School.
Year 1 begins with M0 – Foundations of Medicine, a 4 week course intended to bring the class up to speed in key topics such as cell biology, biochemistry, genetics, microbiology, and how they intertwine in the function of the human body.
The remainder of Year 1 is mostly M1 – Human Biology and Health, which is broken down into several systems-based courses that focus on normal anatomy and physiology.
M2 – Health and Disease follows this by revisiting each system’s pathological states and helping students develop a clinical approach to disease. This module is introduced in the final 9 weeks of Year 1 and continues on to represent the majority of Year 2.
Pre-clerkship ends with M3 – Consolidation, a unique 10 week course that allows students to integrate all of the knowledge they have gained, mainly through the use of small group tutorials and assigned studies.
There are also several longitudinal courses that run throughout Pre-clerkship – Clinical Skills, Clinical Reasoning, Indigenous Health, Population Health, and Professionalism.
Pre-clerkship Evaluations
Nearly all pre-clerkship courses have a midterm multiple choice exam at the halfway point, followed by a cumulative final multiple choice exam at the end. This includes most longitudinal courses as well.
Throughout the year, there are also assigned studies, written assignments, and activities with participation marks that must be completed.
One special set of exams are those of the Clinical Skills course – the OSCEs (objective structured clinical examination). OSCEs are designed to evaluate students’ physical examination and history taking skills through the use of standardized patients and scenarios. In Year I there is a 2-station FOSCE (F for formative), followe by 3 more OSCEs (2-, 8-, and 2-station). The pattern in Year II is similar, with 3more OSCEs (2-, 2-, and 8-station). Marks are combined between all 12 stations annually, with the pass mark determined as 90% of the average of the top 10 students’ marks.
Gross Anatomy Labs
Gross anatomy labs often seem intimidating to new medical students. Our curriculum has begun to de-emphasize the dissection portion of these labs, often providing students with prosected specimens to study (i.e. cadavers that have already been dissected and have structures isolated and displayed). The labs also utilize clinical cases and diagnostic imaging in conjunction with the cadaveric specimens to teach human anatomy.
Scrubs or a lab coat are highly recommended; lockers are available outside of the lab. A dissection kit it useful, especially if you plan to go on your own time. Most groups find sharing a kit works well.
These sessions, like others, will be what you make of them – so be respectful and try your best! Remember that most doctors don’t need a thorough understanding of esoteric anatomy to do their day-to-day jobs – and even those surgeons that do may not have enjoyed their very first gross lab. So relax! If you’re looking for a resource, Rohen’s Color Atlas of Anatomy: A Photographic Study of the Human Body is likely the best.
CPAs
CPAs, or Comprehensive Patient Assessments, are designed to be a medical student’s first interaction with real patients. There are several different CPAs to account for the differences between disciplines:
- Family Medicine – A Standardized Patient encounter, similar to an OSCE station. Student encounters are filmed and then reviewed with a family medicine preceptor.
- Surgery – Students shadow surgeons for these CPAs.
- Pediatrics – Students interact with volunteer families in the CLSF under the guidance of a pediatrician.
- Internal Medicine – Students are assigned a patient on the medical teaching wards. They then must go and do a full history and physical examination on said patient, followed by a presentation to an internal medicine attending the next day.
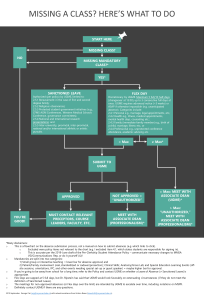
Absences
Summer Opportunities
- B.Sc. (Med) Program – Degree research program consisting of two 13-week terms spread over two summers
- Camp Briardale – Work as part of the medical staff at a Canadian Diabetes Association summer camp located in the Whiteshell; may be applied for Early Exposure credit (see below). Contact Dr. Elizabeth Sellers for more info.
- Home for the Summer – Clinical placements in rural/northern MB communities
- IFMSA Exchanges – Explore clinical or research placements in other countries!
- Northern Medical Unit (NMU) – Clinical placements in First Nations communities. Range from 12 day elective to full 10 week program. Contact Kathy Risk at the Dept of Community Health Sciences
- Summer Early Exposures – Opportunities to gain credited early clinical exposure in a multitude of fields
- WISH Clinic – Work at the Winnipeg Interprofessional Student-run Health Clinic to assist in the provision of after-hours care to the Point Douglas community.
Wellness and Mistreatment
Medical School can be incredibly challenging but it should also be a positive and rewarding experience. You can’t properly learn or care for others if you don’t care for yourself.
Be sure to also take a look at our Wellness page for tips about personal wellness. When in doubt, contact Dr. Aviva Goldberg, Dean of Student Affairs – she’s the best! We at the MMSA are also here for you, please feel free to drop us a line anytime if you’d like to speak with a peer.
Transition to Clerkship
Students are given the opportunity to request specific “Clerkship Tracks”; i.e. which order they will experience their core rotations. This typically occurs near the end of Winter/beginning of Spring of Med II. We encourage students to seek out mentors in upper years for advice regarding the advantages and disadvantages of each Track. Some general topics to consider:
- Rotating through disciplines you are “on the fence” about early, in order to evaluate career interest
- Rotating through disciplines you are keen on later on, in order to better impress attendings/residents
At the end of Med II, you will get to choose your Med III Selectives. In addition to your core clerkship rotations, many rotations allow you to choose a subspecialty to rotate through.
See this spreadsheet for tips and info about various rotations and Selectives and feel free to add your own experiences!
Enjoy your last summer! Med III will begin with Module 4 – Transition to Clerkship, a 5 week period that uses tutorials, simulations, and real patient encounters to acclimate students to the clinical duties and scenarios that they will soon find themselves in. It ends with one week of shadowing on each student’s first core rotation.
